ventilator-associated pneumonia (VAP)
Last edited 06/2021 and last reviewed 06/2021
Hospital acquired pneumonia occurs mostly in patients who are severely debilitated or who are immune suppressed.
Hospital-acquired pneumonia (HAP) is a respiratory infection developing more than 48 h after hospital admission.
- HAP affects 0.5% to 1.0% of inpatients and is the most common healthcare-associated
infection (HCAI) contributing to death
- estimated to increase hospital stay by 7-9 days
- in a proportion of patients, HAP is associated with mechanical ventilation,
in which case it is termed ventilator-associated pneumonia (VAP)
- in patients with VAP, there is a 24% to 50% mortality rate - increases to 76% if infection is caused by multidrug-resistant pathogens
- VAP accounts for up to 25% of all intensive care unit (ICU) infections
- risk being highest during early ICU stay when it is estimated to
be 3%/day during the first 5 days of ventilation
- followed by 2%/day up to day 10 of ventilation and thereafter 1%/day
- risk being highest during early ICU stay when it is estimated to
be 3%/day during the first 5 days of ventilation
Most common organisms isolated from respiratory specimens of patients known or suspected to have HAP are Pseudomonas aeruginosa, Staphylococcal aureus and Enterobacteriaceae (especially Klebsiella, E. coli and Enterobacter spp.)
- polymicrobial cultures are common in VAP, occurring in up to 60% of the case studies with anaerobes and fungi being uncommon.
- longer a patient is in hospital, the wider the spectrum of likely pathogens and the more likely they are to be multiple drug resistant.
- early-onset HAP or VAP
- often caused by typical antimicrobial-susceptible community organisms such as Streptococcus pneumoniae or Haemophilus influenzae
- late-onset HAP or VAP
- commonly caused by P. aeruginosa or other antimicrobial-resistant opportunistic Gram-negative bacteria or by MRSA
- note though that there is an increasing frequency of early-onset HAP caused by nosocomial pathogens, probably resulting from recent prior hospitalization and/or antimicrobial therapy
Empirical Antibiotic treatment:
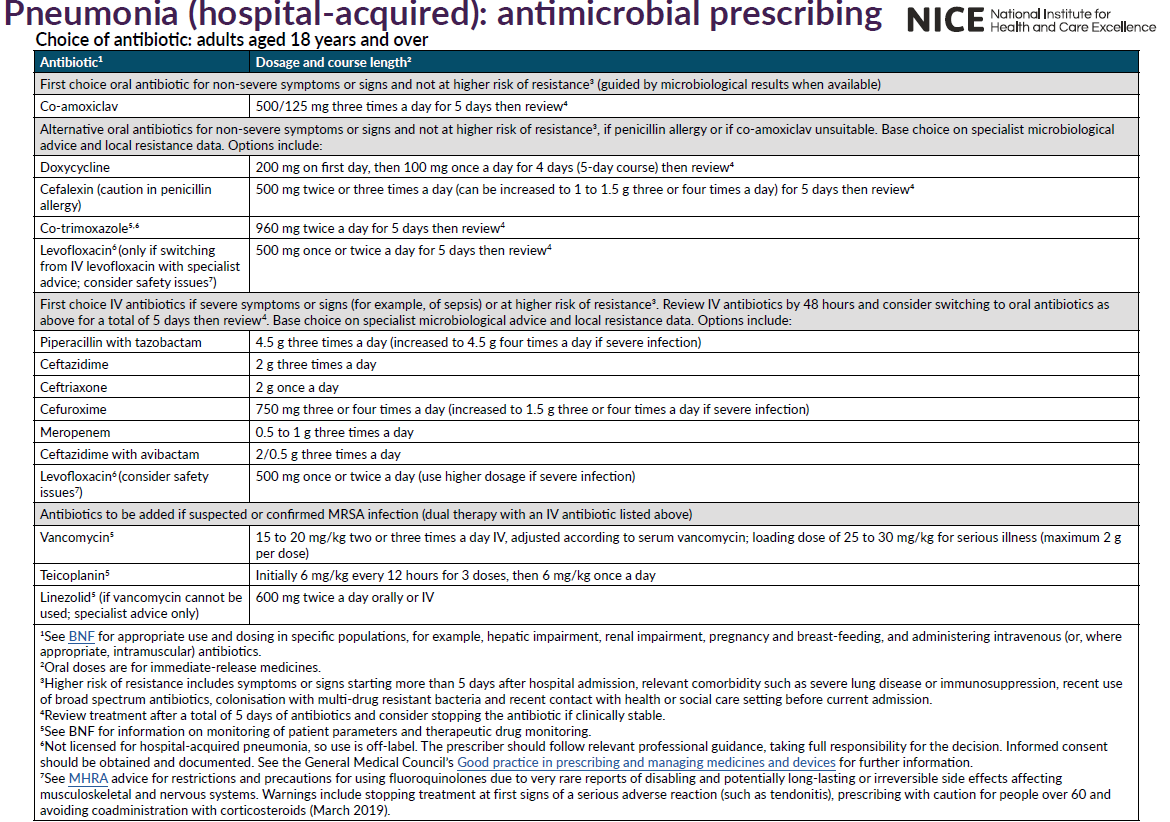
- choice of empirical antibiotic therapy should be based on the knowledge of the nature and susceptibility patterns of the pathogens that are prevalent on that unit and should also take account of such variables as duration of hospital stay (i.e. early- or late-onset infection), recent administration of antibiotic therapy and co-morbidities
- definitive therapy should be determined by culture and susceptibility test results
- for patients with early-onset infections (fewer than 5 days following admission to hospital) who have not previously received antibiotics and in the absence of other risk factors, the use of co-amoxiclav or cefuroxime would be appropriate
- for patients with early-onset infections (fewer than 5 days following admission to hospital) who have recently received antibiotics and/or who have other risk factors, a third-generation cephalosporin (cefotaxime or ceftriaxone), a fluoroquinolone or piperacillin/tazobactam would be appropriate
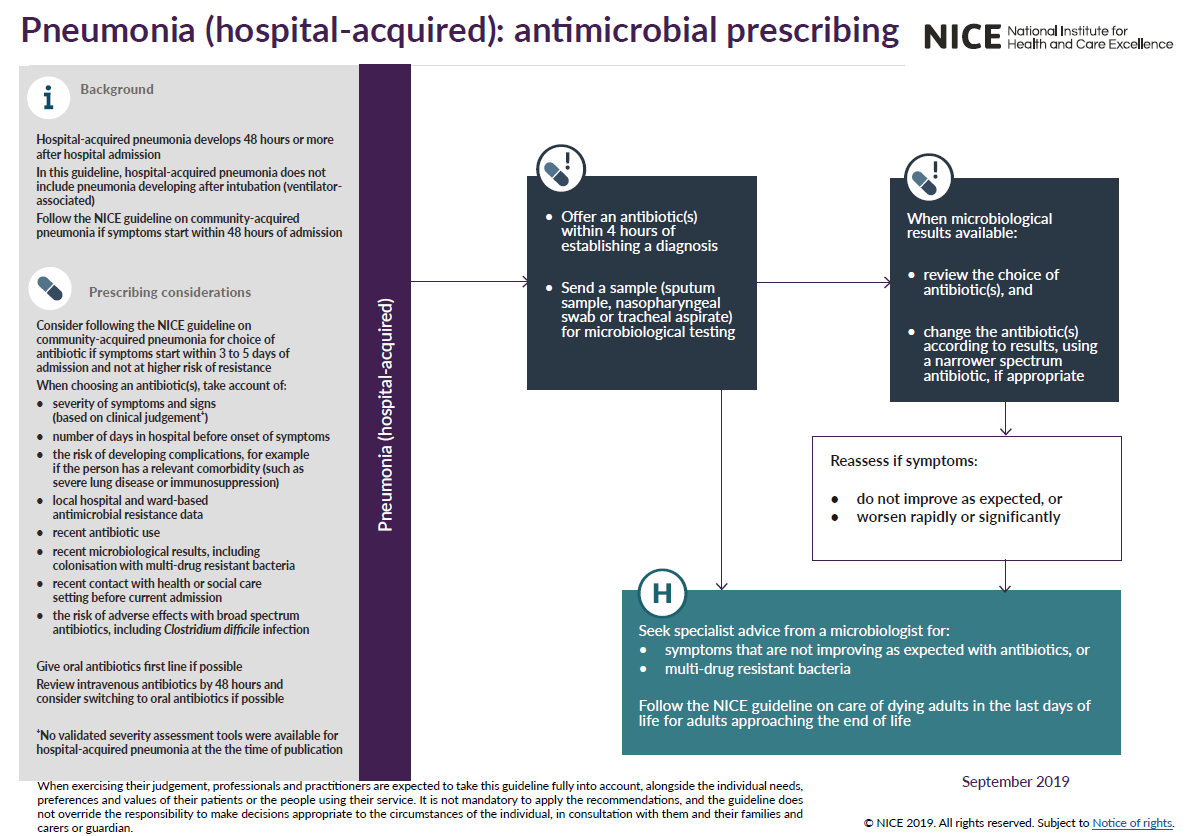
NICE have stated (2):
Notes:
- no proven optimal antibiotic regimen for patients with HAP suspected or proven to be caused by P. aeruginosa. Treatment options include ceftazidime, ciprofloxacin, meropenem and piperacillin/tazobactam
- metronidazole should be used in addition if there is a likelihood of anaerobic infection
Reference:
- Masterton RG et al. Guidelines for the management of hospital-acquired pneumonia in the UK: report of the working party on hospital-acquired pneumonia of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother. 2008 Jul;62(1):5-34.
- NICE (September 2019). Pneumonia (hospital-acquired): antimicrobial prescribing
- Public Health England (June 2021). Managing common infections: guidance for primary care