prognosis
Last edited 06/2019 and last reviewed 07/2022
The main determinants of prognosis for malignant melanoma are the tumour thickness, measured from the overlying granular layer of the epidermis to the deepest easily identifiable tumour cells - the Breslow thickness, and the presence of ulceration of the primary tumour.
In the American Joint Committee on Cancer (AJCC) 2002 Staging system for malignant melanoma (1) there is less significance with respect the level of invasion (Clark's levels) in prognosis. Analysis of histopathologic features of melanoma comparing Clark's level and Breslow's depth have shown that the actual tumour thickness is more predictive of outcome. However there is an instance in which Clark's level invasion continues to carry prognostic information: In patients with 'thin' (<1.0 mm) melanoma, Clark's level IV or V lesion portends a worse prognosis. For this reason, pathologists need to continue to include Clark's level along with tumour thickness and ulceration in the histology report of the primary melanoma
Other prognostic determinants:
- site - back, arms, neck and scalp lesions fair worse
- pathology - worst for nodular, best for lentigo
- sex - worse for males
- age - worsens with age, possibly due to immunological factors or decreased motivation for treatment
- mitotic rate - worse for higher
- tumour volume - more accurate prognosis but difficult to perform
- regression - associated with an unfavourable prognosis for thin tumours
- metastasis - poor if metastasised - 10% 5 year survival
- satellites - metastases occurring at a distance of less than 50mm from the main tumour are a poor prognostic finding
- host inflammatory response - improves prognosis
- immunological factors - increased expression of HLA-DR correlates with worse prognosis as does the ganglioside GD2 on tumour cells
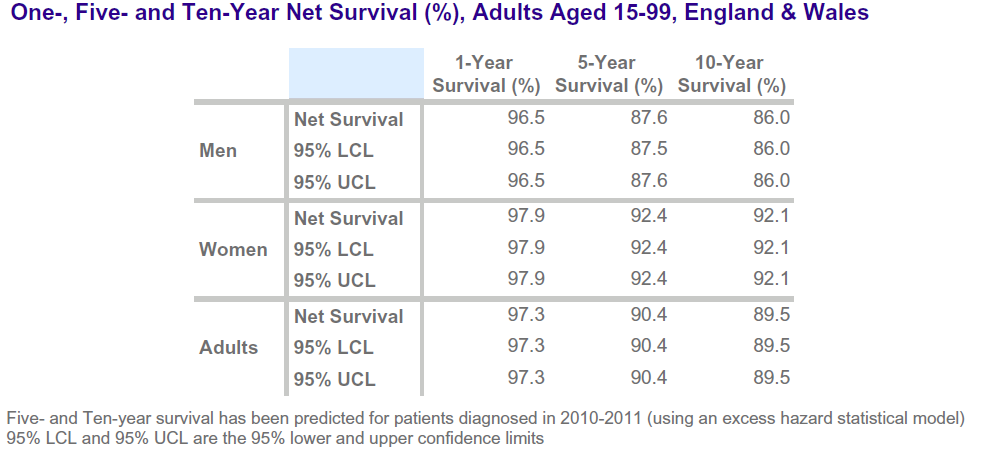
In the UK (2):
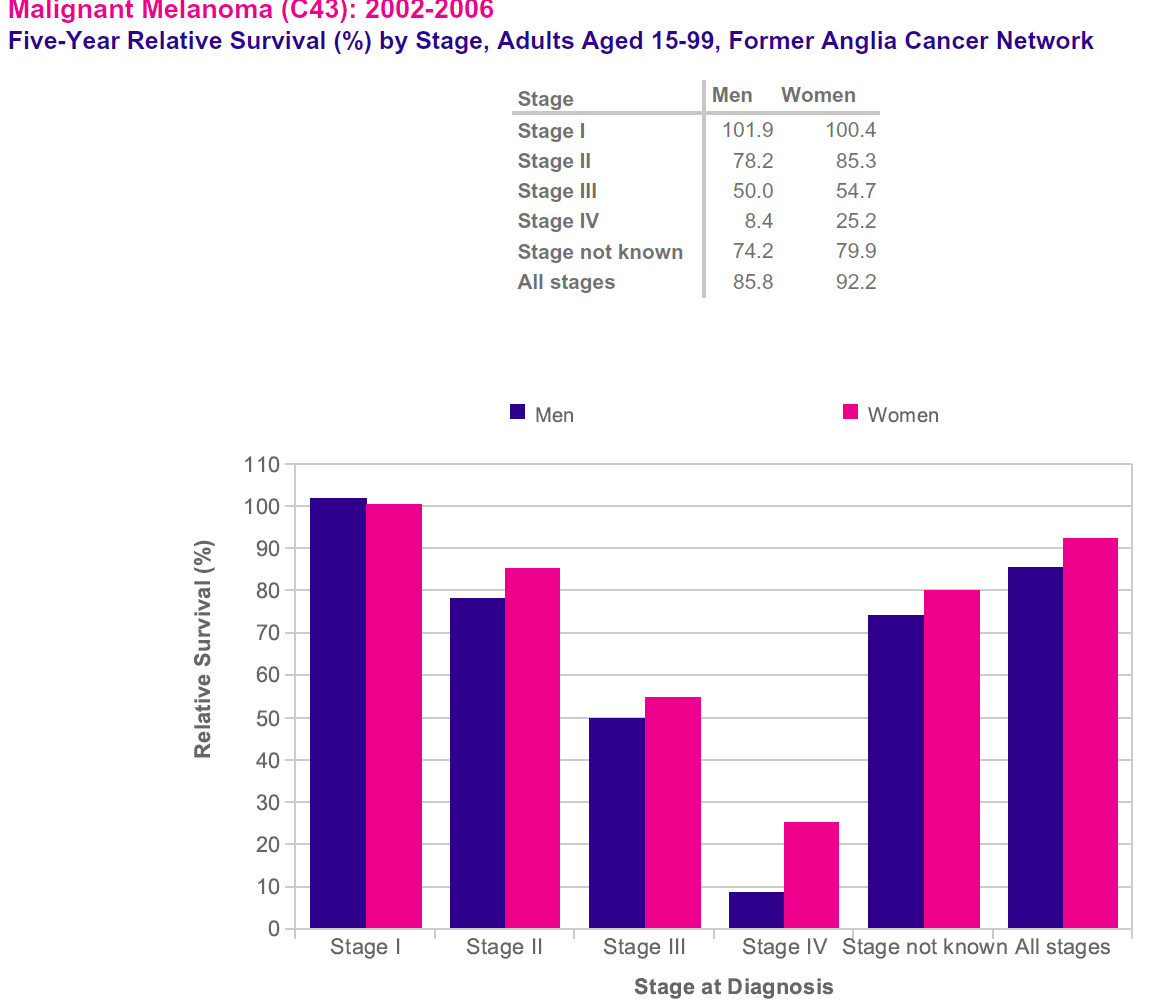
Survival for melanoma skin cancer is strongly related to stage of the disease at diagnosis
- one-year net survival for melanoma skin cancer is highest for patients diagnosed
at stage I, and lowest for those diagnosed at stage IV, 2014 data for England
show. 101% **of patients diagnosed at stage I survived their disease for at
least one year, versus 50% patients diagnosed at stage IV
- note** relative survival can be greater than 100% because it accounts for background mortality and means that people diagnosed have a better chance of surviving after diagnosis than the general population
A study (3) outlined similar factors for poorer prognosis:
- in patients with a first invasive melanoma, tumours of the scalp/neck or trunk, older age, being male, tumour thickness, and ulceration were associated with increased risk of melanoma-specific mortality
Reference:
- 1. Cancer Control. 2002 Jan-Feb;9(1):9-15.
- 2. CRUK. Melanoma Skin Cancer Survical Statistics (Accessed 27/5/19)
- 3. Lachiewicz AM et al. Survival differences between patients with scalp or neck melanoma and those with melanoma of other sites in the Surveillance, Epidemiology, and End Results (SEER) program. Arch Dermatol. 2008 Apr;144(4):515-21.