management
Last edited 03/2020
On presentation to the health professional with a history of infantile colic
- exclude any organic cause for the symptoms, e.g. gastro-oesophageal reflux, constipation, infection, etc.
- the differential includes intestinal obstruction, hernia and febrile illnesses - however there are generally other pointers to these alternative diagnoses
The treatment of this condition is supportive; it usually resolves by about the fourth month of life.
Treatment options include:
- dietary modifications
- prevalence of colic is similar between breastfed and bottle-fed infants, hence breastfeeding should not be discontinued
- hypoallergenic formula preparations for bottle fed infants
- switching to hydrolysed formulas (from partially hydrolysed to completely hydrolysed formula preparations) have shown to reduce colic symptoms
- several studies have reported that use of completely hydrolysed formulas resulted in improved clinical symptoms of infantile colic, such as crying time (when cow’s milk formula was used as the comparator)
- a systematic review stated that benefits reported for hydrolysed formulas were inconsistent (1)
- soybased formulas are not recommended for infantile colic
- hypoallergenic maternal diet for breastfed infants
- a randomized controlled trial reported that breastfed infants of mothers who follow a low-allergen diet, showed significant reduction in colic symptoms (2)
- any maternal dietary modifications should be accompanied by dietary counseling to ensure adequate nutrition
- a review states that any maternal diet modification may result in improving symptoms of colic secondary to undiagnosed cows' milk protein allergy in the infant, rather than infantile colic with no underlying cause (3)
- lactase therapy
- it was suggested that in a significant number of cases, the immediate cause of infantile colic is transient lactose intolerance, in which cases pretreatment of feeds with lactase can result in considerable symptomatic benefits
- galactosidase (lactase) drops are mixed with breast or bottle milk feeds up to 24 hours prior to feeding the infant
- several randomised control trials have reported improvement in symptoms in infants with lactase therapy. This finding is controversial since several other randomised controlled trials noted no improvement with the use of lactase in either breast or formula milk
- there is inconsistent and conflicting evidence on the benefits of lactase drops for the treatment of infantile colic (3)
- pharmacological
- infacol, which contains simethicone (activated dimeticone) - however evidence of benefit is uncertain
- dicycloverine (dicyclomine), because of its adverse effect profile, is now considered unsafe for use in infants under six months (3,4)
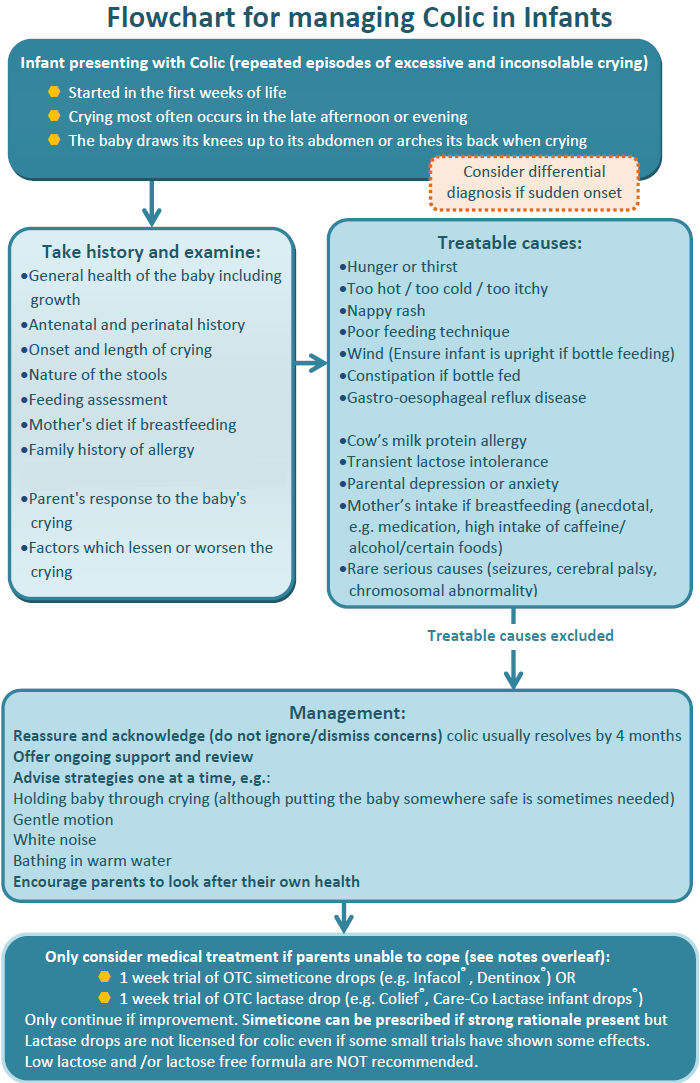
A flowchart for the management of infantile colic has been suggested (6):
Notes:
- probiotics in the management of infantile colic
- there is some evidence that Lactobacillus reuteri improved colicky symptoms in breastfed infants within 1 week of treatment, compared with simethicone - the authors concluded that probiotics may have a role in the treatment of infantile colic (6)
- a review stated that there was insufficient evidence to recommend use of probiotics in infantile colic (1)
Reference:
- (1)Gordon M et al. Dietary modifications for infantile colic. Cochrane Database Syst Rev 2018 Oct 10;10:CD011029.
- (2) Hill DJ et al. Effect of a low-allegen maternal diet on colic among breastfed infants: a randomized, controlled trial. Pediatrics 2005; 116:e 709-15.
- (3) Drug and Therapeutics Bulletin. Management of infantile colic. BMJ. 2013;347:f4102
- (4) Johnson JD, Cocker K, Chang E. Infantile Colic: Recognition and Treatment. Am Fam Physician. 2015;92(7):577-82
- (5) Savino F et al. Lactobacillus reuteri (American Type Culture Collection Strain 55730) versus simethicone in the treatment of infantile colic: a prospective randomized study.Pediatrics. 2007 Jan;119(1):e124-30.
- (6) Wessex Infant Feeding Guidelines and Appropriate Prescribing of Specialist Infant Formulae (Accessed 8/3/2020)