stopping and/or swapping antidepressant treatment
Last edited 04/2023 and last reviewed 06/2023
Stopping antidepressant treatment
- the timing of when to stop antidepressant treatment is discussed in menu item below (length of antidepressant treatment)
- patients should be advised not to stop treatment suddenly or omit doses - patients should also be forewarned about possible symptoms that may occur when treatment is discontinued
- Drug and Therapeutics Bulletin (1) advises:
- after a 'standard' 6-8 months treatment it is recommended that treatment should be tapered off over a 6-8 week period
- if the patient has been on maintenance therapy then an even more gradual tapering e.g. by 1/4 of the treatment dose every 4-6 weeks, is advised
- if a treatment course has lasted less than 8 weeks then discontinuation over 1-2 weeks is considered safe
- this contrasts with the Maudsley prescribing guidelines (2) which recommend
that antidepressants should be withdrawn slowly, preferably over four weeks,
by weekly increments for example,
Drug maintenance dose (mg/day) dose after 1st week (mg/day) dose after 2nd week (mg/day) dose after 3rd week (mg/day) dose after 4th week (mg/day) amitriptyline 150 100 50 25 Nil paroxetine 30 20 10 5 (liquid) Nil trazadone 450 300 150 75 Nil If withdrawal symptoms occur then the rate of drug withdrawal should be slowed or (if the drug has been stopped) the patient should be given reassurance that symptoms rarely last more than 1-2 weeks (2).
- NICE also suggest a four week period for withdrawal of antidepressant
treatment (4):
- stopping or reducing antidepressants
- advise people that discontinuation symptoms may occur on stopping, missing doses or, occasionally, reducing the dose of the drug. Explain that these are usually mild and self-limiting over about 1 week, but can be severe, particularly if the drug is stopped abruptly
- normally, gradually reduce the dose over 4 weeks (this is not necessary with fluoxetine). Reduce the dose over longer periods for drugs with a shorter half-life (for example, paroxetine and venlafaxine)
- advise the person to see their practitioner if they experience significant
discontinuation symptoms. If symptoms occur:
- monitor them and reassure the person if symptoms are mild
- consider reintroducing the original antidepressant at the dose that was effective (or another antidepressant with a longer half-life from the same class) if symptoms are severe, and reduce the dose gradually while monitoring symptoms
- for detailed guidance then consult the full guideline (4)
- stopping or reducing antidepressants
Swapping antidepressant treatment (2):
- when swapping from one antidepressant
to another, abrupt withdrawal should usually be avoided. Cross-tapering is preferred,
where the dose of the ineffective or poorly tolerated drug is slowly reduced while
the new drug is slowly introduced for example,
week 1 week 2 week 3 week 4 withdrawing dosulepin 150 mg od 100mg od 50 mg od 25 mg od Nil introducing citalopram Nil 10 mg od 10mg od 20 mg od 20 mg od
Vortioxetine switching (3)
- vortioxetine is a new antidepressant and there is limited experience when switching, therefore extra caution is required, particularly when switching to or from inhibitors of CYP2D6, such as fluoxetine and paroxetine
- when switching to another antidepressant, doses above 10mg should be reduced to 10mg over a period of 7 days before stopping and starting the new antidepressant
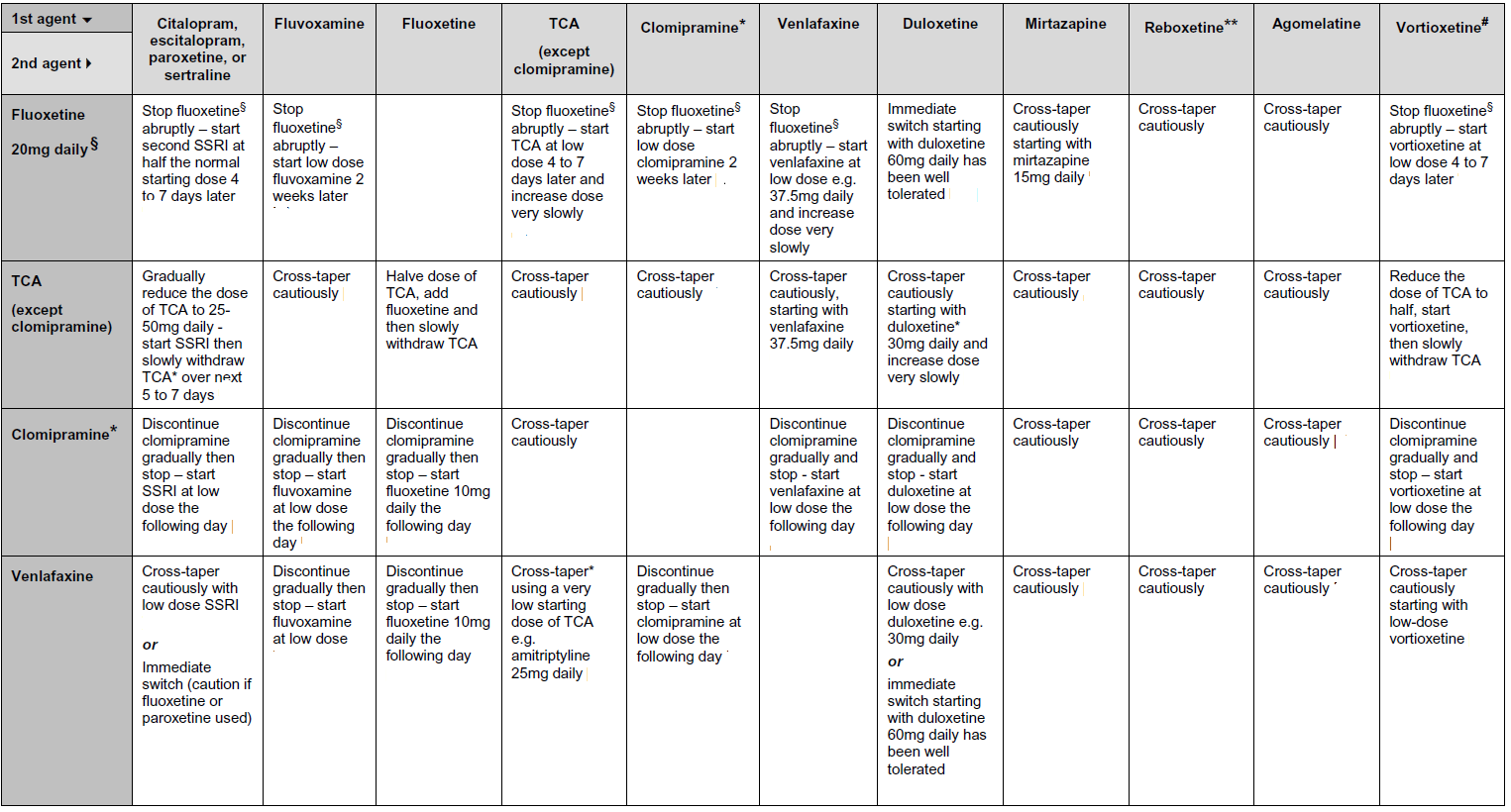
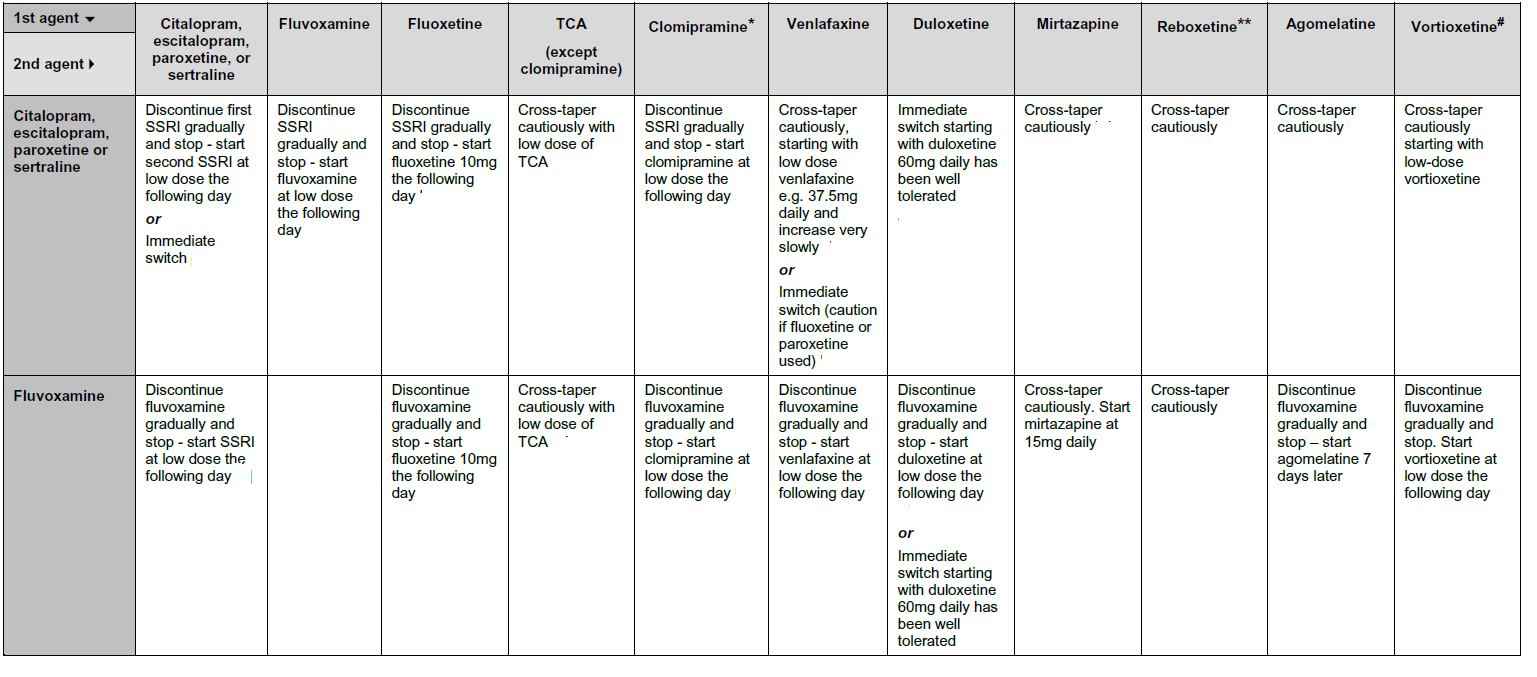
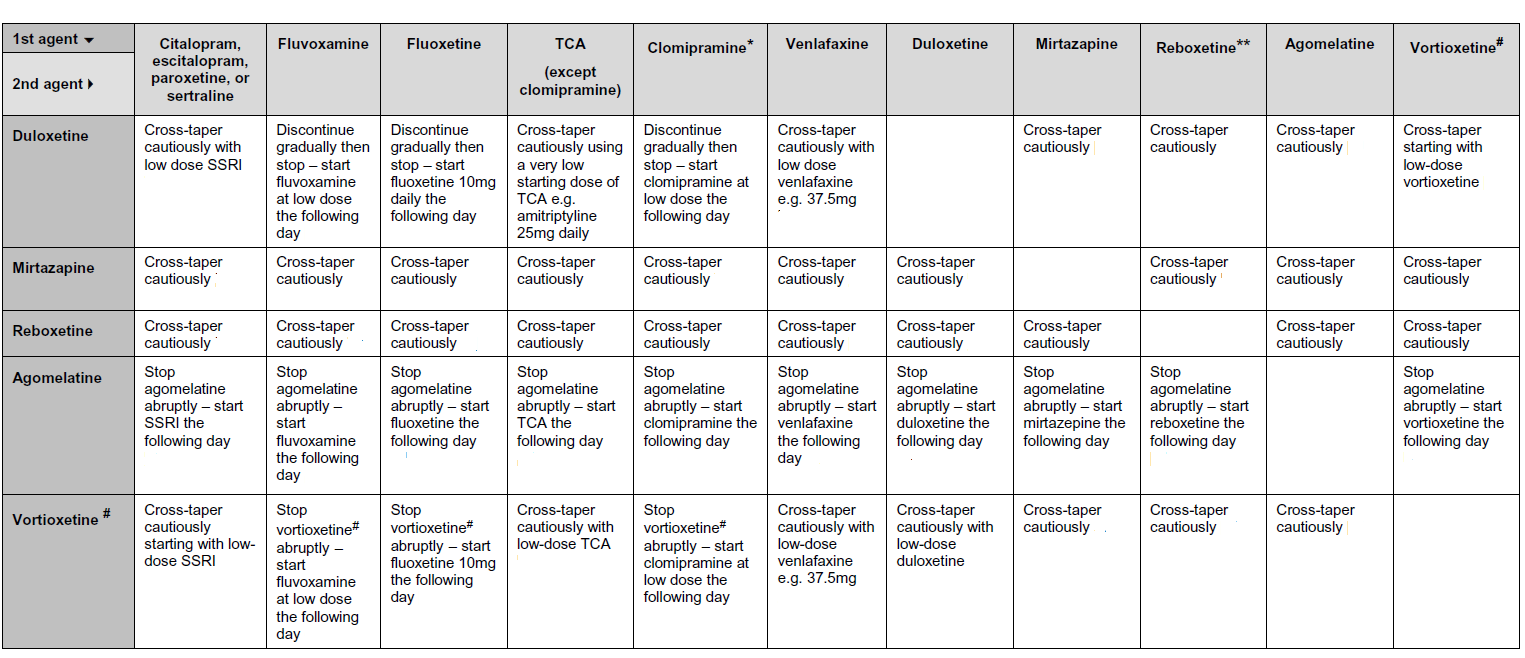
Antidepressant use: swapping and stopping
The tables below have been adapted from the Maudsley prescribing guidelines (2,3). However it is recommended that local prescribing guidelines and/or specialist psychiatric advice must be consulted when swapping antidepressant medication. Also the specific summary of product characteristics for each of the antidepressants involved should be consulted. It has been noted that there are no clear guidelines on switching antidepressants, so caution is required (2).
Table showing switching from either:
- fluoxetine 20mg per day, or
- a tricyclic antidepressant, or
- clomipramine, or
- venlfaxine
to an alternative antidepressant
Table showing switching from either:
- citalopram, escitalopram, paroxetine or sertraline; OR
- fluvoxamine
to an alternative antidepressant
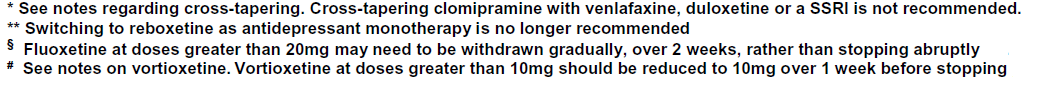
Table showing switching from either:
- duloextine, OR,
- mirtazapine, OR,
- reboxetine, OR,
- agomelatne, OR,
- vortioxetine
to an alternative antidepressant
NICE guidance regarding switching antidepressants is less detailed (4):
- do not switch to, or start, dosulepin
- because evidence supporting its tolerability relative to other antidepressants is outweighed by the increased cardiac risk and toxicity in overdose
- when switching to another antidepressant, which can normally be achieved
within 1 week when switching from drugs with a short half life, consider the
potential for interactions in determining the choice of new drug and the nature
and duration of the transition. Exercise particular caution when switching:
- from fluoxetine to other antidepressants, because fluoxetine has a long half-life (approximately 1 week)
- from fluoxetine or paroxetine to a TCA, because both of these drugs inhibit the metabolism of TCAs; a lower starting dose of the TCA will be required, particularly if switching from fluoxetine because of its long half-life
- to a new serotonergic antidepressant or MAOI, because of the risk of serotonin syndrome
- from a non-reversible MAOI: a 2-week washout period is required (other antidepressants should not be prescribed routinely during this period).
Notes:
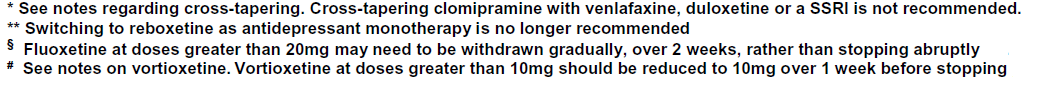
- do not co-administer clomipramine and SSRIs or venlafaxine
- when switching between one SSRI and another, some consider cross-tapering
the doses generally not to be necessary (6,7)
- selective serotonin reuptake inhibitors (SSRIs) overlap in their mechanism of action, and the new SSRI will usually prevent discontinuation symptoms that may occur when the first SSRI is stopped. Substituting a new SSRI at the relatively equivalent dose of the former SSRI is typically well-tolerated , though starting the new SSRI at a lower dose may also be considered since patients occasionally have idiosyncratic side effects to particular SSRIs (5)
- the New Zealand formularly guidance (6) supports no need for cross-tapering
for switching between short acting SSRIs (citalopram, escitalopram, paroxetine,
sertraline) - but for switches from fluoxetine then it supports the Maudsley
guidance and states
- stop fluoxetine, wait 4 - 7 days, start SSRI at low dose (low dose= citalopram 10mg/day; escitalopram 5mg/day; paroxetine 10mg/day; sertraline 25mg/day)
- the effects of the first SSRI are likely to be so similar to that of
the second one, that the second SSRI will reduce the discontinuation effects
of the first (2). The abrupt switch between SSRIs may still produce discontinuation
symptoms, and vigilance is still advised. In cases where discontinuation
symptoms arise a short period of dose tapering is recommended before starting
a different SSRI
- * withdrawal effects may be more pronounced. Slow withdrawal over 1-2 months may be necessary
Reference:
- Drug and Therapeutics Bulletin (1999); 37 (7):49-52.
- The Maudsley Prescribing Guidelines 2001; 6th Ed, p64 - 65.
- UKMi (NHS). How do you switch between tricyclic, SSRI and related antidepressants? (November 2015)
- NICE (April 2018). Depression
- MIMS - Switching and Withdrawing Antidepressants (Accessed 6/8/13).
- UptoDate - Antidepressant medication in adults: Switching and discontinuing medication (Accessed 6/8/13)
- Using the New Zealand Formulary : Guide for switching antidepressants (Accessed 6/8/13)
discontinuation syndromes with antidepressants
length of treatment/continuation of antidepressant treatment
stopping or switching treatment with an SSRI
NICE guidance - management of depression in primary and secondary care
considerations when etablishing whether a person needs to switch their antidepressant
considerations when choosing an antidepressant to switch to
summary advice - switching from tricyclic antidepressants (TCAs) to another antidepressant
summary advice - switching from vortioxetine to another antidepressant
summary advice - switching from mirtazapine to another antidepressant