investigations
Last edited 12/2019 and last reviewed 11/2023
Measles is a clinical diagnosis. (although in UK this has a low positive predictive value since the incidence of measles is low) (1)
In Summary:
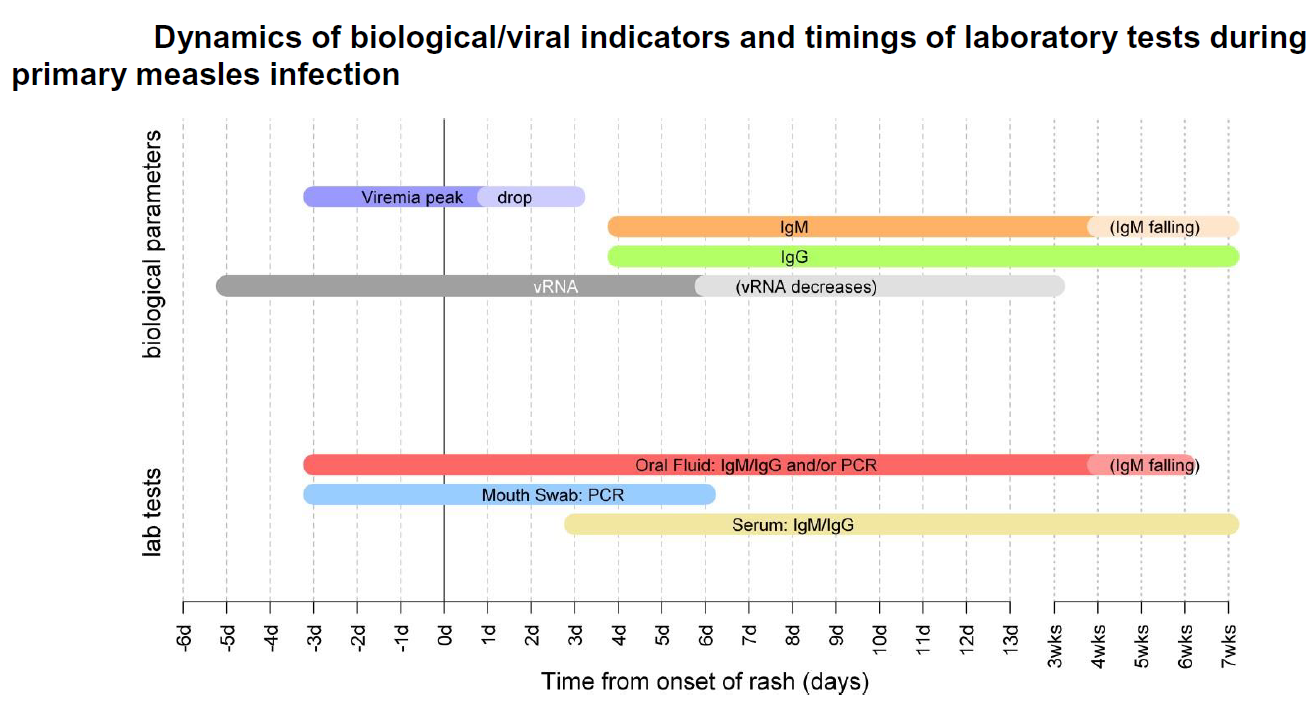
Diagnosis should be confirmed by laboratory testing in suspected cases (1). The following non-invasive methods can be used:
- salivary swab for measles specific IgM taken within six weeks of onset or
- serum sample for measles specific IgM taken within six weeks of onset or
- RNA detection in salivary swabs or other samples (1)
In Detail:
Measles is a single-stranded RNA virus (genus Morbillivirus, family paramyxoviridae)
- are 24 described genotypes, many of which have been eliminated as part
of the global control of measles. Less than 10 genotypes are currently found
globally, the distribution of which varies across geographic areas
- genotyping on confirmed samples is an integral part of laboratory surveillance
for measles, to identify imported cases and monitor progress towards elimination
- oral fluid (OF) is the optimal sample for measles surveillance
- these samples are minimally invasive and are more acceptable than serum
for confirming cases in infants and children. Importantly, OF can be tested
for IgM, IgG and measles RNA, and can therefore:
- i) reliably exclude measles diagnosis, as well as confirm it;
- ii) indicate whether the case is primary or breakthrough measles (reinfection);
- and iii) genotype confirmed cases.
Oral fluid
- oral fluid (OF) is the optimal sample for measles surveillance and should
be taken from all suspected cases regardless of any other samples that may
have already been taken, including when other laboratory methods have not
confirmed measles
- OF can be tested for both measles IgM/IgG using specific enzyme immunoassays
(EIA), and viral RNA using specifically designed assays. Testing for IgM on
OF is more sensitive and more specific than serum, particularly in the first
few days after the rash, as IgM antibodies are positive in >50% of samples
on day one of the rash, and in over 90% by day 3 of the rash .For oral fluid
samples taken within 7 days of onset of disease, PCR analysis for RNA detection
is also performed (2)
- OF can be tested for measles IgG, and although measles IgG avidity is not
done on OF samples, the relative level of measles IgG can be used to predict
whether the case is a primary or re-infection with measles
- measles viral RNA can be detected from before the onset of the rash and
for at least 2 weeks after the onset of symptoms. Genotyping for molecular
epidemiology can be performed on PCR positive samples, which allows the characterisation
of the virus into one of the 24 known genotypes, and help identify clusters
and imported cases
- measles genotyping also allows the distinction between wild-type virus
and vaccine in those developing a measles-like rash following vaccination
- it is important to note that oral fluid samples cannot be used to assess the immune status of vulnerable contacts and serum should be used instead
Serum
- serum samples can be used for IgM/IgG detection through enzyme immunoassays
(EIA)
- serum is the most appropriate sample to assess the immune status of contacts
- serum samples may still be IgM negative within 3 days of onset of rash -
this may be longer for IgM assays used in some laboratories - the timing of
the sample in relation to rash onset is therefore essential to properly interpret
results
- serum can be used to confirm breakthrough measles (reinfection) by detection
of high avidity measles IgG
- serum is not suitable for PCR detection and viral typing
- serum cannot be used to distinguish wild-type measles from vaccine-derived measles following recent vaccination
Mouth swabs
- mouth swabs can be used for PCR if collected within 6 days of the onset
of rash. A negative PCR result does not exclude a diagnosis of measles
- mouth swabs can be used to distinguish between wild-type virus and vaccine
in someone who has recently been vaccinated
- mouth swabs cannot be used to distinguish between a primary infection and a breakthrough measles (reinfection)
Throat swabs/Nasopharyngeal Aspirate/Urine/EDTA blood
- such samples can be used for PCR if collected within 6 days of the onset of rash
- such samples are less suitable than the others mentioned and generally not advisable for measles testing (2)
Reference:
- (1) Asaria P, MacMahon E. Measles in the United Kingdom: can we eradicate it by 2010? BMJ. 2006;333(7574):890–895
- (2) Public Health England (November 2019). National measles guidelines.