low libido in a man
Last reviewed 03/2023
Libido
- libido relates to a person's desire for sexual activity and sex seeking
behaviour
- levels of libido vary from person-to-person, and there is considerable individual variation, with libido changing across relationships as well in different social and environmental circumstances
- low libido becomes a problem when it creates distress for the patient and/or their partner and difficulty across the relationship
- unrealistic perceptions about male libido may strongly influence a man's feelings of shame and embarrassment if they experience low sex drive (1)
Assessment and management
Loss of libido is a not uncommon presenting symptom in general practice and can be affected by many factors including:
- fatigue - such as from long or irregular working hours
- stressors - from any source, but potentially related to work, finances, health or relationships
- lack of psychological wellbeing - such as depression, anxiety or low self esteem
- relationship problems - such as conflict, poor intimacy or sexual incompatibility
Systematic questioning is required to elicit symptoms in these areas, as loss of libido may need to be judged 'by the company it keeps'.
While there may be some reduction in a man's libido with ageing (as in menopausal women) this is by no means universal
Reduction in libido to discordant levels in either partner may negatively impact the relationship in terms of dissatisfaction and conflict, which could lead to the partner seeking alternative relationships
While low libido is more commonly the result of psychosocial factors, other causes must be excluded
- biological causes (eg. testosterone deficiency, diabetes, thyroid disorders
and other endocrinopathies)
- reduced libido is widely considered the most prominent symptomatic reflection
of low testosterone levels in men
- testosterone deficiency (TD) afflicts approximately 30% of
men aged 40-79 years, with an increase in prevalence strongly associated
with aging and common medical conditions including obesity, diabetes,
and hypertension
- decreased libido is a concern often expressed by aging patients,
it is difficult to measure comprehensively, being multifactorially
determined and associated with both psychosocial and organic factors
- phenomenon of hypogonadism due to aging has also been described
as testosterone deficiency syndrome, late-onset hypogonadism
(LOH), and andropause
- symptoms of this condition resemble those of 'normal' aging and include changing body composition (osteopenia, increased adiposity, decreased muscle mass), decline in energy and stamina, decreased cognitive function, decreased libido, and erectile dysfunction, systolic hypertension, carotid artery-wall thickness, increased abdominal visceral-fat mass, insulin resistance, reduced HDL concentrations, postprandial somnolence, impaired quality of life and depressive mood
- phenomenon of hypogonadism due to aging has also been described
as testosterone deficiency syndrome, late-onset hypogonadism
(LOH), and andropause
- testosterone levels in men begin to decline in the late third
or early fourth decade and diminish at a constant rate thereafter
- no universal agreement regarding the exact definition of
hypogonadism. However, it is generally accepted that hypogonadism
refers to the presence of persistently low circulating testosterone
compared with the normal range derived from healthy young
and middle-aged men. This range is approximately 10.4-34.7
nmol/L in most assays of serum total testosterone, although
wide variation may exist between different commercial assays
(2)
- a suggested algorithm for assessment of possible testosterone
deficiency is (3):
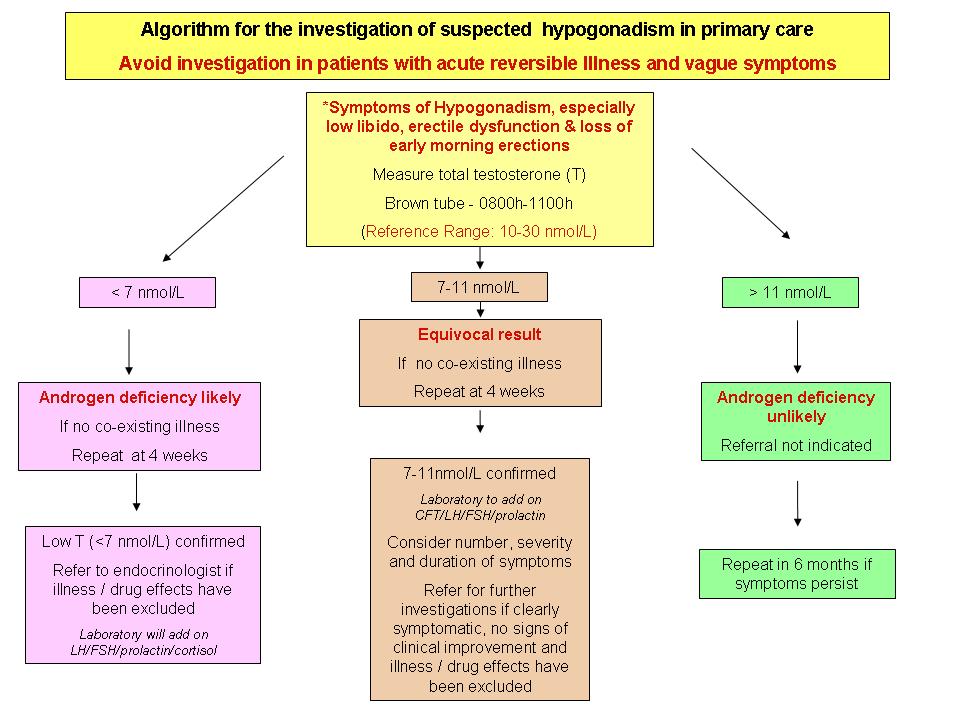
- The algorithm above is based on common clinical features and an early morning (8-11am) serum testosterone
- Illness and certain drugs can modify testosterone levels - consider as confounding factors prior to referral
- NB: Older (especially obese) men may have borderline
testosterone levels: Evidence of replacement therapy
is conflicting (and possibly harmful) and probably
has little role for symptoms that are not discriminant
such as fatigue. Referral is unlikely to be of benefit
- Key points:
- investigate only once any acute illness
has fully resolved
- most discriminant symptoms associated with
low testosterone (<11nmol/L) are: low libido,
loss of early morning erections & erectile
dysfunction - particularly in combination
- consider endocrine referral if suggestive
clinical symptoms + chronic androgen deficiency
ie TWO early am (8-11am) testosterone samples
<11 nmol/L at least 4 weeks apart:
- Refer if repeat sample <7nmol/L or those in the 7-11 range having clear hypogonadal symptoms
- If repeat sample 7-11 nmol/L and no
clear symptoms: consider reversible causes
(drug/illness)
- further monitoring after several months
may be appropriate
- investigate only once any acute illness
has fully resolved
- confounding, potentially reversible factors
affecting testosterone. Concurrent illness, certain
drugs (prescribed or otherwise) and lifestyle
factors (e.g. excessive alcohol; stress; possibly
weight gain/obesity) can all potentially cause
reversible hypogonadism (low testosterone) or
contribute to symptoms
- Key points:
- a suggested algorithm for assessment of possible testosterone
deficiency is (3):
- no universal agreement regarding the exact definition of
hypogonadism. However, it is generally accepted that hypogonadism
refers to the presence of persistently low circulating testosterone
compared with the normal range derived from healthy young
and middle-aged men. This range is approximately 10.4-34.7
nmol/L in most assays of serum total testosterone, although
wide variation may exist between different commercial assays
(2)
- decreased libido is a concern often expressed by aging patients,
it is difficult to measure comprehensively, being multifactorially
determined and associated with both psychosocial and organic factors
- testosterone deficiency (TD) afflicts approximately 30% of
men aged 40-79 years, with an increase in prevalence strongly associated
with aging and common medical conditions including obesity, diabetes,
and hypertension
- reduced libido is widely considered the most prominent symptomatic reflection
of low testosterone levels in men
- iatrogenic causes (eg. medications such as SSRIs, antipsychotics and beta-blockers)
- lifestyle (eg. excessive alcohol use)
Erectile dysfunction, while not necessarily a cause of low libido, may result in sexual avoidance behaviour that ultimately leads to loss of libido.
While reduction in libido is a manifestation of depression, the treatment of depression using some SSRIs may also complicate this symptom by further exacerbating low libido and/or potentially creating difficulties in reaching orgasm (anorgasmia)
Management may include information, counselling, and being mindful of the libido-reducing side effects of some medications
- if testosterone deficiency then seek expert advice re: management as described
above
- testosterone supplementation may be advised
- there is evidence that Tradamixina (2) (150 mg of Alga Ecklonia Bicyclis, 396 mg of Tribulus Terrestris and 144 mg of D-Glucosamine and N-Acetyl-D-Glucosamine) for two months improved libido in elderly men. In this trial daily tadalafil improved erectile dysfunction but had no affect libido
Reference:
- 1) Wijesinha S, Piterman L, Kirby CN. The male reproductive system - An overview of common problems. Aust Fam Physician. 2013 May;42(5):276-8.
- 2) Iacono F et al.Sexual asthenia: Tradamixina versus Tadalafil 5 mg daily. BMC Surg. 2012;12 Suppl 1:S23.
- 3) Refhelp - Investigation of suspected hypogonadism in primary care (accessed July 10th 2013)
testosterone supplementation in older men
Kisspeptin in Hypoactive Sexual Desire Disorder (HSDD) in men