PPI and stomach cancer risk
Last edited 01/2023 and last reviewed 02/2023
PPI and gastric cancer risk:
Abbas et al undertook a review (1) concerning PPI use and gastric cancer risk:
- two nationwide based studies were included in this review, the Cheung study
(2), and the Brusselaers study (3)
- Cheung study included a total of 63,397 individuals, where 153 cases developed gastric cancer. PPI users had a hazard ratio of 2.44 (95% confidence interval [CI] 1.42-4.20), and the risk of cancer increased with the duration of PPI use
- Brusselaers study included a total of 797,067 individuals, where 2,219
cases developed gastric cancer
- standardized incidence ratio of gastric cancer among PPI users was 3.38 (95% CI 3.23-3.53), and the risk of cancer increased with the duration of PPI use
- Abbas et al concluded that chronic PPI use is associated with an increase in the risk of gastric cancer. It might also be an independent risk factor for gastric cancer
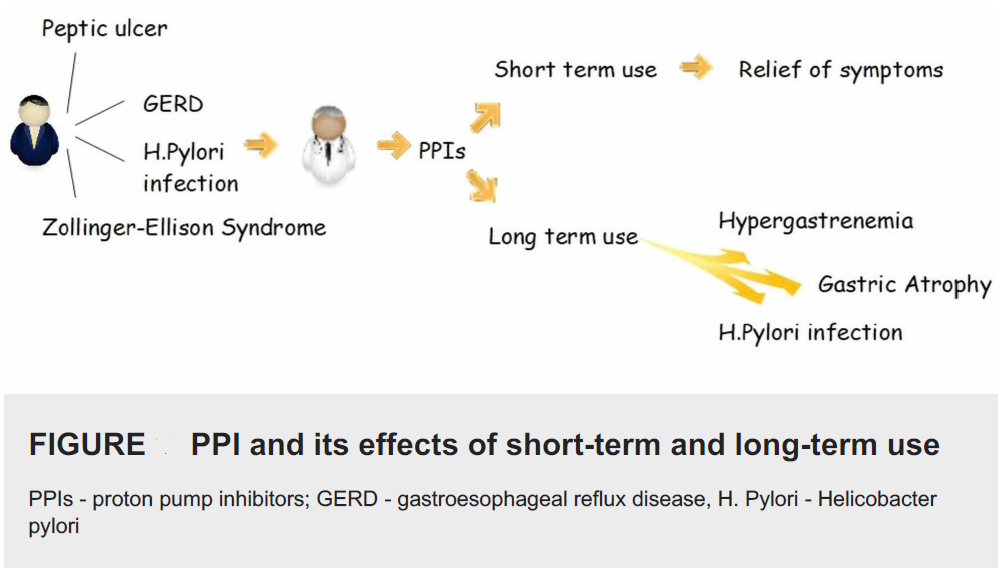
The dilemma we are facing is that although PPIs are used to treat patients with hypergastrinaemia and H. pylori infection, in the long run, they cause hypergastrinaemia and H. pylori infection (1):
- some local effects of long term PPIs use include atrophic gastritis due to prolonged acid suppression, hypergastrinemia, chronic H. pylori infection, and development of gastric polyps
- gastric cancer risk is considerably high among individuals infected with H. pylori who are susceptible to the development of corpus atrophy (2)
- PPIs stimulate the production of gastrin, which is a potent growth factor, and hypergastrinemia has been shown to induce hyperplasia of enterochromaffin-like cells (2)
- all four local effects are risk factors for gastric cancer (1)
Cheung and Leung have stated:
- gastric cancer remains one of the leading cancers in the world with a high
mortality, particularly in East Asia
- Helicobacter pylori infection accounts for the majority of the noncardia gastric cancers by triggering gastric inflammation and subsequent neoplastic progression. Eradication of H. pylori can reduce, but not totally eliminate, subsequent risk of developing gastric cancer
- Proton-pump inhibitors (PPIs) with their profound gastric-acid suppression,
there are concerns about a possible carcinogenic role in gastric cancer,
due to induced hypergastrinemia, gastric atrophy and bacterial overgrowth
in the stomach
- while randomized clinical trials to establish causality between long-term PPI use and gastric cancer are lacking, current evidence based on observational studies suggests PPIs are associated with an increased gastric cancer risk
- however, opinions on causality remain divergent due to unmeasured and possible residual confounding in various studies
- our recent study has showed that even after H. pylori eradication (2) , long-term PPI use is still associated with an increased risk of gastric cancer by more than twofold. Hence, long-term PPIs should be used judiciously after considering individual's risk-benefit profile, particularly among those with history of H. pylori infection
- further well-designed prospective studies are warranted to confirm the potential role of PPIs in gastric cancer according to baseline gastric histology and its interaction with other chemopreventive agents like aspirin, statins and metformin
Piovani et al (5):
- systematically searched Medline/PubMed, Embase and Scopus databases (until June 1, 2022) for randomised and non-randomised studies (NRS) of the association between PPIs and gastric cancer having considered Histamine-2 receptor antagonists (H2RAs) users as controls
- the study authors stated that they chose this comparison to minimise confounding by indication, and focus on patients requiring gastric acid suppression
- found no association between PPIs and gastric cancer in NRS having adequately controls
Reference:
- Abbas MK et al. The Safety of Long-term Daily Usage of a Proton Pump Inhibitor: A Literature Review.Cureus. 2019 Sep 4;11(9):e5563
- Cheung KS et al. Long-term proton pump inhibitors and risk of gastric cancer development after treatment for Helicobacter pylori: a population-based study.Gut. 2018 Jan;67(1):28-35
- Brusselaers N et al. Maintenance therapy with proton pump inhibitors and risk of gastric cancer: a nationwide population-based cohort study in Sweden. BMJ Open. 2017 Oct 30;7(10):e017739
- Cheung KS, Leung MK. Long-term use of proton-pump inhibitors and risk of gastric cancer: a review of the current evidence.Therap Adv Gastroenterol. 2019 Mar 11;12
- Piovani, D et al. Meta-analysis: Use of proton pump inhibitors and risk of gastric cancer in patients requiring gastric acid suppression. Aliment Pharmacol Ther. 2022; 00: 1-13. https://doi.org/10.1111/apt.17360