follow-up pharmacological treatment
Last edited 02/2021 and last reviewed 05/2021
A separate algorithm is provided for FOLLOW-UP treatment, where the management is still based on symptoms and exacerbations, but the recommendations do not depend on the patient’s GOLD group at diagnosis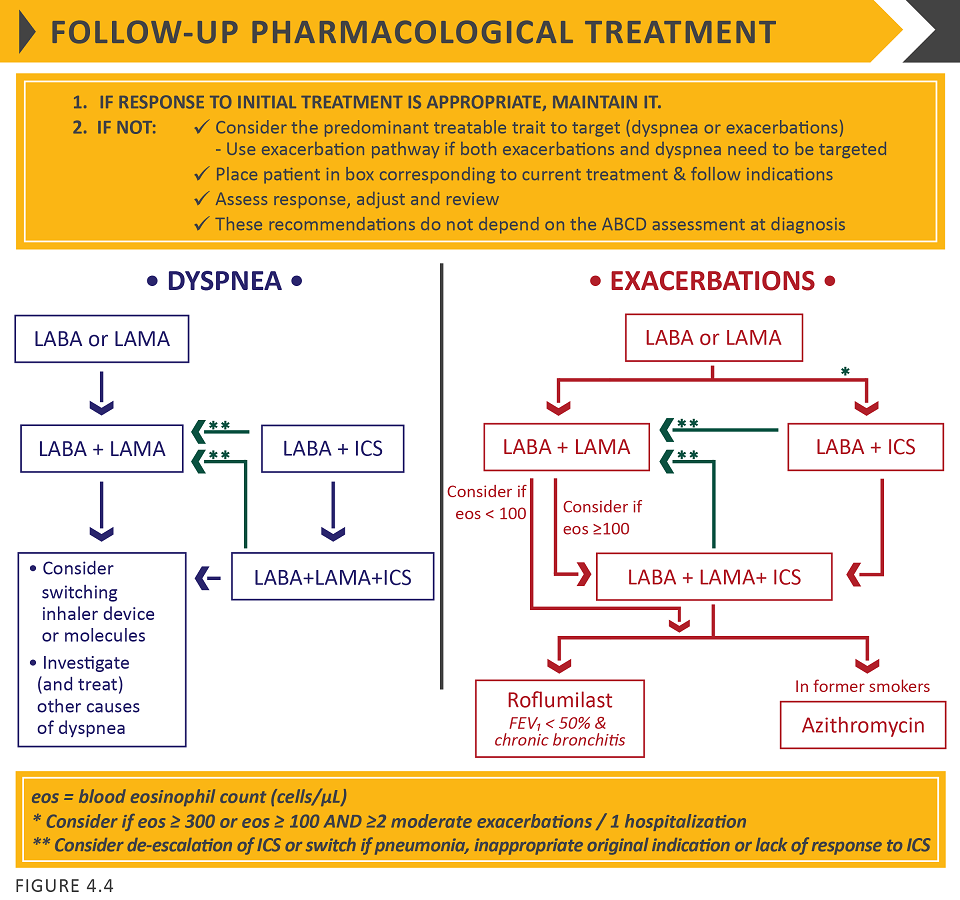
© 2020, Global Initiative for Chronic Obstructive Lung Disease, available from www.goldcopd.org, published in Fontana, WI, USA.
The Figure above suggests escalation and de-escalation strategies based on available efficacy as well as safety data
The response to treatment escalation should always be reviewed, and de-escalation should be considered if there is a lack of clinical benefit and/or side effects occur.
De-escalation may also be considered in COPD patients receiving treatment who return with resolution of some symptoms that subsequently may require less therapy.
Patients, in whom treatment modification is considered, in particular de-escalation,should be undertaken under close medical supervision.
GOLD authors note that they are fully aware that treatment escalation has not been systematically tested; trials of de-escalation are also limited and only include ICS.
Follow-up pharmacological management
- The follow-up pharmacological treatment algorithm can be applied to any patient who is already taking maintenance treatment(s) irrespective of the GOLD group allocated at treatment initiation
- the need to treat primarily dyspnoea/exercise limitation or prevent exacerbations further should be evaluated.
- if a change in treatment is considered necessary then select the corresponding algorithm for dyspnoea ( left column) or exacerbations (, right column); the exacerbation algorithm should also be used for patients who require a change in treatment for both dyspnoea and exacerbations. Identify which box corresponds to the patient's current treatment
Follow up pharmacological management should be guided by the principles of first review and assess, then adjust if needed:
Review
- Review symptoms (dyspnoea) and exacerbation risk.
Assess
- Assess inhaler technique and adherence, and the role of non-pharmacological approaches (covered later in this chapter).
Adjust
- Adjust pharmacological treatment, including escalation or de-escalation. Switching inhaler device or molecules within the same class (e.g. using a different long acting bronchodilator) may be considered as appropriate. Any change in treatment requires a subsequent reviewof the clinical response, including side effects.
Dyspnoea
- for patients with persistent breathlessness or exercise limitation on long-acting bronchodilator monotherapy, the use of two bronchodilators is recommended:
- if the addition of a second long acting bronchodilator does not improve symptoms, GOLD suggests the treatment could be stepped down again to monotherapy. Switching inhaler device or molecules can also be considered
- for patients with persistent breathlessness or exercise limitation on LABA/ICS treatment, LAMA can be added to escalate to triple therapy:
- alternatively, switching from LABA/ICS to LABA/LAMA should be considered if the original indication for ICS was inappropriate (e.g. an ICS was used to treat symptoms in the absence of a history of exacerbations), or there has been a lack of response to ICS treatment, or if ICS side-effects warrant discontinuation
- alternatively, switching from LABA/ICS to LABA/LAMA should be considered if the original indication for ICS was inappropriate (e.g. an ICS was used to treat symptoms in the absence of a history of exacerbations), or there has been a lack of response to ICS treatment, or if ICS side-effects warrant discontinuation
- at all stages, dyspnoea due to other causes (not COPD) should be investigated and treated appropriately. Inhaler technique and adherence should be considered as causes of inadequate treatment response.
Exacerbations
- for patients with persistent exacerbations on long-acting bronchodilator monotherapy, escalation to either LABA/LAMA or LABA/ICS is recommended.
- LABA/ICS may be preferred for patients with a history or findings suggestive of asthma
- Blood eosinophil counts may identify patients with a greater likelihood of a beneficial response to ICS
- for patients with one exacerbation per year, a peripheral blood level >=300 eosinophils/mul identifies patients more likely to respond to LABA/ICS treatment
- for patients with >=2 moderate exacerbations per year or at least one severe exacerbation requiring hospitalisation in the prior year, LABA/ICS treatment can be considered at blood eosinophil counts >=100 cells/mul, as ICS effects are more pronounced in patients with greater exacerbation frequency and/or severity
- in patients who develop further exacerbations on LABA/LAMA therapy GOLD suggests two alternative pathways. Blood eosinophil counts < 100 cells/muL can be used to predict a low likelihood of a beneficial ICS response:
- escalation to LABA/LAMA/ICS. A beneficial response after the addition of ICS may be observed at blood eosinophil counts >=100 cells/mul, with a greater magnitude of response more likely with higher eosinophil counts, or,
- add roflumilast or azithromycin (see below) if blood eosinophils <100 cells/mul
- escalation to LABA/LAMA/ICS. A beneficial response after the addition of ICS may be observed at blood eosinophil counts >=100 cells/mul, with a greater magnitude of response more likely with higher eosinophil counts, or,
- in patients who develop further exacerbations on LABA/ICS therapy, GOLD recommends escalation to triple therapy by adding a LAMA. Alternatively, treatment can be switched to LABA/LAMA if there has been a lack of response to ICS treatment, or if ICS side effects warrant discontinuation
- in patients treated with LABA/LAMA/ICS who still have exacerbations the following options may be considered:
- add roflumilast. This may be considered in patients with an FEV1 <50% predicted and chronic bronchitis, particularly if they have experienced at least one hospitalisation for an exacerbation in the previous year
- add a macrolide. The best available evidence exists for the use of azithromycin, especially in those who are not current smokers. Consideration to the development of resistant organisms should be factored into decision-making
- stopping ICS. This can be considered if there are adverse effects (such as pneumonia) or a reported lack of efficacy. However, a blood eosinophil count >=300 cells/mul identifies patients with the greatest likelihood of experiencing more exacerbations after ICS withdrawal and who subsequently should be followed closely for relapse of exacerbations
- add roflumilast. This may be considered in patients with an FEV1 <50% predicted and chronic bronchitis, particularly if they have experienced at least one hospitalisation for an exacerbation in the previous year
Reference: